Learn the Facts
Opioids
Opioids are a class of drugs that include prescription pain relievers, heroin, and synthetic opioids like fentanyl. They work by binding to opioid receptors in the brain to reduce pain but also create feelings of euphoria. While effective for pain management, opioids have a high potential for addiction and overdose.

Opioid pain relievers can lead to
Common Forms & Use
Prescription opioids
Used for pain relief; common types include oxycodone (OxyContin), hydrocodone (Vicodin), morphine, and codeine
Heroin
An illegal opioid derived from morphine, typically injected, snorted, or smoked
Synthetic opioids (e.g., fentanyl)
Up to 50 times stronger than heroin and 100 times stronger than morphine; often mixed into other drugs without the user’s knowledge
Illicit opioid pills
Counterfeit prescription medications containing unknown amounts of fentanyl, making them extremely dangerous
Did you know?
Overdose deaths involving opioids have skyrocketed, with synthetic opioids (mainly fentanyl) being the leading cause
In recent years, nearly 75% of drug overdose deaths in the U.S. involved an opioid
Many individuals with opioid use disorder started with legally prescribed painkillers before transitioning to illicit substances
Youth and young adults are increasingly exposed to fentanyl-laced drugs via social media and counterfeit pills
Harm reduction strategies, including naloxone distribution and fentanyl test strips, have been introduced to combat the crisis
Signs of Use
Drowsiness, confusion, and slowed breathing
Pinpoint pupils and nodding off mid-conversation
Track marks or burns
Withdrawal symptoms when not using the drug
Social withdrawal, financial problems, or frequently changing doctors to access prescriptions
What’s the Danger?
Respiratory depression, leading to fatal overdose
Physical dependence and withdrawal, including severe pain, vomiting, and cravings
Increased risk of infections, including HIV and hepatitis, from needle use
Cognitive impairment, leading to memory issues and poor decision-making
Mental health effects, including depression and increased suicide risk
Industry & Marketing Tactics
Pharmaceutical companies downplayed the addictive potential of prescription opioids, leading to overprescribing
The black market for counterfeit pills has surged, with deadly fentanyl-laced versions widely available
Illicit online sales and social media drug markets target youth and young adults
Some street opioids are mixed with xylazine (a veterinary sedative), making overdoses harder to reverse
Treatment access remains a challenge, despite increased efforts for medication-assisted treatment (MAT) and harm reduction programs
Fentanyl
Fentanyl is a powerful synthetic opioid that is 50-100 times stronger than morphine. It is prescribed for severe pain management but is also illegally manufactured and mixed with other drugs, making it extremely dangerous. Even a tiny amount can cause a fatal overdose. Fentanyl affects the central nervous system, causing pain relief, drowsiness, confusion, euphoria, nausea, and respiratory depression.

You cannot
Common Forms & Use
Fentanyl can be found in both prescription and illicit forms:
Prescription Forms
Patches, lozenges, pills, or injections (used for severe pain, such as in cancer patients)
Illicit Forms
Powder, pills, or liquid, often mixed with heroin, cocaine, or fake prescription pills, making it undetectable without test strips
Counterfeit Pills
Fake versions such as, but not limited to, Xanax, Oxycodone, or Percocet that contain fentanyl without the user's knowledge
Did you know?
Fentanyl is the leading cause of overdose deaths in the U.S.
In 2022, synthetic opioids (mostly fentanyl) were involved in 70% of all overdose deaths
Drug dealers mix fentanyl into other substances because it is cheap and highly addictive
Rainbow fentanyl has been designed in bright colors to resemble candy, raising concerns for youth exposure
Social media platforms have become a hub for illegal fentanyl sales, targeting young users
Signs of Use
Pinpoint pupils, slow breathing, and loss of consciousness
Blue lips, fingernails, or pale, clammy skin (signs of overdose)
Needle marks or burnt aluminum foil (signs of injection or smoking fentanyl)
Extreme drowsiness, confusion, and difficulty staying awake
Unexplained missing or altered prescription medications
What’s the Danger?
Extreme drowsiness, confusion, and sedation
Severe respiratory depression, leading to suffocation
High risk of overdose, even with a small amount
Coma and death
Long-term use leads to tolerance, addiction, and withdrawal symptoms
Overdose & Harm Reduction
Naloxone (Narcan) can reverse fentanyl overdoses if administered quickly
Test strips can detect fentanyl in drugs, but awareness and access remain limited
Harm reduction strategies include safe-use education and access to addiction treatment
Many people overdose without knowing they took fentanyl, as it is often mixed into other drugs
Stimulants
Stimulants are a class of drugs that increase brain activity, leading to heightened alertness, energy, and euphoria. They affect the central nervous system by boosting dopamine and norepinephrine levels, which can lead to addiction and long-term health issues.

Stimulants are
Common Stimulants Include
Prescription medications (Adderall, Ritalin, Concerta)
Cocaine and crack cocaine
Methamphetamine (meth)
Synthetic stimulants (bath salts, flakka, gravel)
Caffeine and nicotine (milder stimulants but still habit-forming)
Common Forms & Use
Stimulants can be consumed in various ways:
Pills & Capsules
Prescription stimulants (Adderall, Ritalin, Concerta)
Snorting
Cocaine, crushed prescription stimulants (Adderall, Ritalin, Concerta), synthetic stimulants (bath salts, flakka, gravel)
Smoking
Crack cocaine, methamphetamine, nicotine, synthetic stimulants (bath salts, flakka, gravel)
Injecting
Methamphetamine, dissolved prescription stimulants (Adderall, Ritalin, Concerta), synthetic stimulants (bath salts, flakka, gravel)
Drinking
Energy drinks, excessive caffeine intake
Did you know?
Prescription stimulant misuse is rising, particularly among high school and college students
Methamphetamine use has increased, with highly potent forms becoming more widespread
Cocaine use has returned to rates seen in the 1980s and 1990s
Energy drinks and high-caffeine products are widely used, often leading to stimulant dependence
Polysubstance use (mixing stimulants with other drugs) is becoming more common, increasing overdose risks
Signs of Use
Increased energy and talkativeness
Reduced appetite and rapid weight loss
Dilated pupils and excessive sweating
Irritability, mood swings, or paranoia
Presence of drug paraphernalia (pipes, straws, pill bottles, syringes)
What’s the Danger?
Cardiovascular strain (increased risk of heart attack and stroke)
Mental health disorders, including severe anxiety, paranoia, and psychosis
Physical deterioration, including extreme weight loss and dental decay (meth mouth)
High overdose potential, especially when mixed with opioids or alcohol
Severe withdrawal symptoms, including depression, fatigue, and intense cravings
Industry & Marketing Tactics
Pharmaceutical companies can downplay risks of prescription stimulants, potentially leading to widespread over prescription
Illicit stimulant manufacturers produce increasingly potent drugs, making them more addictive and dangerous
Energy drinks and caffeine products are aggressively marketed, often targeting youth
Drug dealers cut stimulants with dangerous additives such as fentanyl and xylazine, increasing overdose risks
Social media glorifies stimulant use, particularly in high-performance environments (academics, athletics, nightlife culture)
Medications
Commonly Misused Medications
While medications are essential for treating various conditions, some are frequently misused, leading to harmful effects. Commonly misused over-the-counter (OTC) and prescription drugs include:
Over-the-Counter (OTC) Drugs:
Cough syrups and pills (containing dextromethorphan or DXM)
Antihistamines and decongestants (used in high doses for sedation or stimulant effects)
Sleep aids (diphenhydramine-based products like Benadryl, Unisom)
Weight loss medications (stimulant-based diet pills)
Laxatives (misused for weight control, leading to dehydration and electrolyte imbalances)
Prescription Drugs
Opioids (pain relievers like oxycodone, hydrocodone, morphine)
Stimulants (ADHD medications like Adderall, Ritalin, Concerta)
Benzodiazepines (anti-anxiety medications like Xanax, Valium, Ativan)
Sedatives & Sleep Medications (Ambien, Lunesta)
These are
Warning Signs of Misuse
Recognizing medication misuse early can help prevent dependency and overdose. Signs may include:
Taking higher doses or more frequently than prescribed
Doctor shopping to obtain multiple prescriptions
Unexplained drowsiness, confusion, or mood swings
Stealing or frequently borrowing medication
Physical dependence, withdrawal symptoms when stopping use
What’s the Danger?
Misusing medications—whether taking more than prescribed, using someone else’s prescription, or mixing with other substances—can lead to serious consequences, including:
Impaired cognitive and motor functions, increasing accident risk
Increased heart rate, high blood pressure, and nausea from stimulant and decongestant misuse
Respiratory depression and overdose from opioids and sedatives
Psychological effects, including paranoia, agitation, or depression
Addiction and withdrawal symptoms with prolonged misuse
Safe Medication Practices
To prevent misuse and potential harm, follow these key guidelines:
Follow directions on the drug label
Always take the prescribed or recommended dose.
Consult a pharmacist or doctor
Ask about interactions and side effects.
Organize and track medication use
Use a medication log or pill organizer.
Keep medications in a secure location
Store them out of reach of children and others who might misuse them.
Dispose of medications properly
Use drug take-back programs or follow FDA disposal guidelines.
Proper Storage and Disposal
Properly Store Medications
When receiving prescription medications, it is important that you organize and keep track of them. It’s also a good idea to secure any controlled substances that have been prescribed to you and could be misused. These include medications such as hydromorphone (Dilaudid®), oxycodone (OxyContin® and Percocet®), hydrocodone (Vicodin®), alprazolam (Xanax®), lisdexamfetamine (Vyvanse®), amphetamine/dextroamphetamine salts (Adderall®), and methylphenidate (Ritalin®).
As a prescription holder or the guardian of one, you play a big role in keeping these powerful medications out of the hands of those who shouldn’t have them. A locked storage area can help keep others from accessing these substances. By keeping track of and locking away your medications, you are helping prevent an accidental injury and the possible abuse of prescription medications by others.
Medication Drop Boxes
Medication take-back programs are a good way to safely dispose of most unneeded medications.
The U.S. Drug Enforcement Administration (DEA) and our local law enforcement agencies host biannual Prescription Drug Take-Back events (typically in April and October) where collection sites are set up in our local communities for safe disposal of prescription drugs.
Several local law enforcement agencies also have medication drop boxes that can be accessed during regular business hours. Additionally, most pharmacies will take leftover medications and safely dispose of them; call your pharmacy ahead of time to ensure they can take them for you. For more information, please contact your local law enforcement agency.

Industry & Marketing Tactics
Pharmaceutical companies and the healthcare system have played a role in medication misuse:
Aggressive opioid marketing contributed to the opioid crisis
Over prescription of stimulants has led to widespread misuse among students
Misleading OTC drug branding promotes the belief that medications are always safe
Social media trends encourage off-label drug use for weight loss, performance enhancement, or self-medication
Marijuana
Marijuana, also known as cannabis, is a psychoactive drug that affects brain function. It contains tetrahydrocannabinol (THC), the primary compound responsible for its mind-altering effects. Cannabidiol (CBD) is another compound found in marijuana that does not produce a high but is often marketed for medicinal use.
The marijuana of today
Common Forms & Use
Marijuana is consumed in several ways, including:
Smoking
(joints, blunts, bongs)
Vaping
(concentrates, THC oil, cartridges)
Edibles
(THC-infused food and drinks)
Tinctures & Oils
(used sublingually or in cooking)
Topicals
(lotions, balms, patches for localized relief)
Dabbing
(high-potency cannabis extracts like wax and shatter)
Did you know?
Marijuana use has increased, especially among young adults and in states where it is legal
High-potency cannabis products have become more common, with THC levels far exceeding those found in marijuana from previous decades. In fact, today there is no plant form with less than 18% THC. In previous decades, including the 1990’s THC levels were only about 1-3%
Medical marijuana legalization has expanded, but recreational use remains controversial
Adolescent use remains a concern, as early exposure is linked to cognitive and emotional development issues
Edibles and vaping have surged in popularity, leading to accidental overdoses and hospitalizations
Virginia Marijuana Laws Effective July 1, 2021
We all may have varying opinions about marijuana legalization and whether it is safe for medical purposes. However, we can all agree that it is not safe for a young person’s developing brain.

Illegal for anyone under 21 to consume, purchase, or possess any amount
Illegal to use while driving
Illegal to consume in public or on school property
Illegal for anyone to possess more than an ounce
Illegal to distribute, sell, or possess any amount
Signs of Use
Bloodshot eyes, dry mouth, and increased appetite
Impaired coordination and slowed reaction time
Distorted sense of time and paranoia
Mood changes, anxiety, or increased lethargy
Presence of marijuana paraphernalia (vape pens, rolling papers, edibles, etc.)
What’s the Danger?
Cognitive impairment, particularly in teens and young adults
Increased risk of psychosis and schizophrenia in vulnerable individuals
Respiratory issues from smoking or vaping and cardiovascular risks
Impaired memory, perception, and problem-solving
Increased heart rate, anxiety, and coordination issues (risking accidents)
Potential addiction and long-term cognitive impairment
Higher risk of mental health disorders (depression, anxiety, schizophrenia)
Dependency and withdrawal symptoms, including mood swings and irritability
Accidental overdose risks with edibles due to delayed effects and varying serving sizes
THC potency has increased significantly, making today's marijuana much stronger than in the past
As the laws change and accessibility increases, the unintended message may be that legal=safe
Cannabinoid hyperemesis syndrome (CHS): Episodes of vomiting, nausea, stomach pain, and dehydration
Industry & Marketing Tactics
Edibles, vape pens, and flavored products are designed to appeal to younger consumers
Marketing portrays marijuana as natural and harmless, downplaying potential risks
Celebrity endorsements and social media normalize and glamorize use
Medical claims often lack regulation, leading to misinformation about benefits and risks
Nicotine
Nicotine is a highly addictive stimulant found in tobacco products and vaping devices. When consumed, it rapidly enters the bloodstream and affects the brain, creating a temporary sense of relaxation and alertness. However, nicotine also disrupts brain development, particularly in young users, impairing cognitive function, attention, and memory. It increases the risk of anxiety, depression, and addiction to other substances.
Nicotine
Common Forms & Use
Nicotine is found in several forms, including:
Cigarettes
Traditionally the most common method of nicotine consumption
Vaping devices (e-cigarettes)
The most popular nicotine product among youth, often marketed as a "safer" alternative
Chewing tobacco (dip, snuff, pouches)
Smokeless but still harmful, leading to gum disease and oral cancers
Cigars & Hookahs
Contain high nicotine levels and produce harmful smoke
Nicotine pouches & lozenges
Emerging products promoted as smoke-free alternatives, but still addictive and damaging to health
Did you know?
Vaping has been the most-used tobacco product among youth since 2014
Many vaping devices now use salt nicotine, which delivers higher doses more smoothly, increasing addiction potential
Cigarette smoking has declined, but the tobacco industry continues to market new nicotine products to maintain sales
Signs of Use
Increased irritability, anxiety, or restlessness
Frequent coughing or shortness of breath
Use of vape devices, cigarettes, or nicotine pouches
Yellowed fingers or teeth (from smoking)
Withdrawal symptoms like headaches and difficulty concentrating
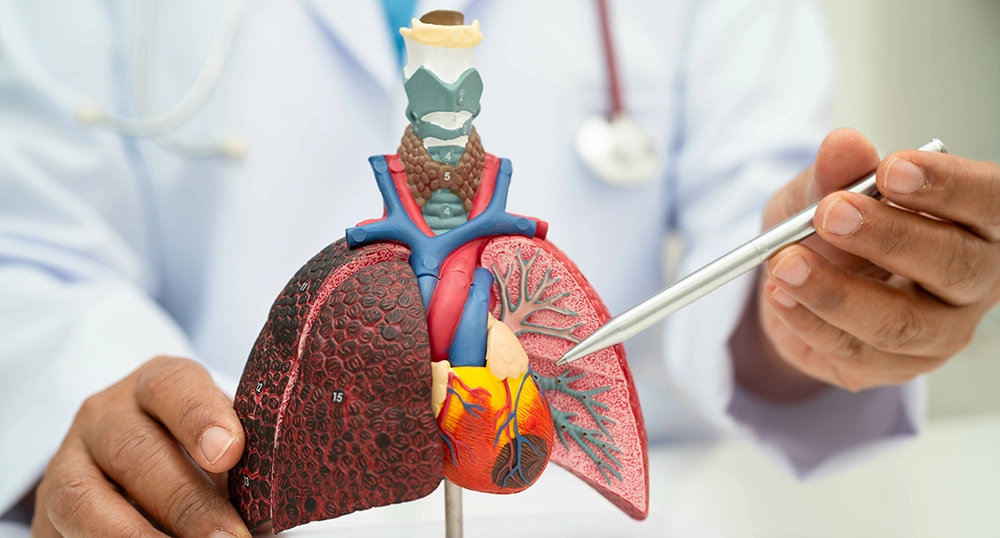
What’s the Danger?
Raises blood pressure and heart rate, increasing the risk of heart disease and stroke
Damages lungs, leading to chronic bronchitis, emphysema, and EVALI
Increases the risk of cancer (lung, throat, esophageal)
Causes gum disease, mouth sores, and digestive issues with smokeless nicotine products
Industry & Marketing Tactics
As cigarette use declined, the tobacco industry aggressively marketed vapes and smokeless nicotine as safer alternatives with little long-term research
Bright packaging, enticing flavors, and sleek designs make nicotine products more appealing, particularly to youth
Misinformation downplays health risks, using terms like “tobacco-free nicotine” to create a false sense of safety
Disposable vapes make it easier for young users to hide their addiction and avoid detection

A message from your local Heroic. Young. Powerful. Energetic (HYPE) Club
Your local HYPE Club invites you to join them by sharing this important information with your friends and loved ones, so we aren’t made to be a guinea pig for vape companies! To learn more about the harmful ingredients in vapes and other toxic substances, we invite you to keep reading!
Help us spread the word by sharing these videos on your social media.
Alcohol
Alcohol is a depressant that slows down brain function and impairs judgment, coordination, and reaction time. It affects the central nervous system, leading to short-term effects like relaxation, lowered inhibitions, and impaired thinking.
Common Forms & Use
Alcohol comes in various forms, including:

Beer
Typically contains 4-6% alcohol by volume (ABV)
Liquor
(spirits like vodka, whiskey, rum, tequila) – Contains a higher ABV, usually 35-50%
Wine
Generally has an ABV of 12-15%
Mixed drinks & cocktails
Can vary widely in alcohol content
Flavored alcohol & alcopops
Sweetened beverages that appeal to younger consumers
Did you know?
Excessive alcohol use is the third leading preventable cause of death in the U.S.
1 in 6 adults binge drinks: consuming 4+ drinks (for women) 5+ drinks (for men) in about 2 hours
Underage drinking rates have declined, but binge drinking remains a concern among teens and young adults
Alcohol-related liver disease has risen significantly, especially in young adults
Marketing targets youth with social media promotions, flavored alcohol products, and normalization of heavy drinking in media
Signs of Use
Slurred speech, unsteady movements, and impaired coordination
Frequent hangovers or needing alcohol to function
Risky behaviors, including drunk driving or unsafe sexual activity
Mood swings, aggression, or depression
Hiding or lying about drinking habits
What’s the Danger?
Impaired judgment leading to accidents, injuries, and risky behavior
Liver damage, including cirrhosis and fatty liver disease
Heart disease, high blood pressure, and stroke risk
Mental health decline, including depression and increased suicide risk
Alcohol poisoning, which can be fatal with excessive consumption
Industry & Marketing Tactics
Alcohol companies market flavored drinks, social media ads, and sponsorships to appeal to young consumers
Messaging promotes alcohol as a way to relax, socialize, and fit in, downplaying risks
Ads highlight partying and fun while omitting long-term consequences
Alcohol can be easily accessible, with few barriers for underage users to obtain it
Some alcohol brands promote “healthier” options like organic or low-calorie alcohol to reduce perceived harm
Remembering Cade Bailey
“Never in a million years did I think I would be in a position that ended up killing my best friend.”
Overdose Response
Know How to Save a Life!
Why Carry Naloxone?
Naloxone (Narcan) is a life-saving medication that can quickly reverse the effects of an opioid overdose, restoring normal breathing within minutes. It is safe, easy to use, and has no effect if opioids are not present in the system.

Why is Naloxone Important?
Opioid overdoses can happen to anyone. Even those who use prescription opioids as directed or those unintentionally exposed to fentanyl are at risk.
Fast action saves lives. Brain damage and death can occur within minutes of an overdose, but naloxone can reverse the effects in time for emergency medical help to arrive.
Fentanyl is widespread. Many illicit drugs, including counterfeit pills and stimulants, are laced with fentanyl, increasing overdose risks.
It’s easy to use. Available as a nasal spray or injection, naloxone can be administered by anyone, including friends, family, and bystanders.
It has no harmful effects. No concerns about harm if given to someone who is not experiencing an opioid overdose.
Recognizing and Responding to an Opioid Overdose
Opioid overdoses can be fatal but knowing the signs and acting quickly can save a life. Common signs include:
Slow, shallow, or no breathing
Unresponsiveness or unconsciousness
Blue or grayish lips and fingernails
Gurgling or choking sounds
Pinpoint pupils
Steps to Respond to an Opioid Overdose
1. Check for responsiveness
- Shake the person gently and shout their name.
- If there’s no response, rub your knuckles firmly on their sternum.
2. Call 911 immediately
- Give the dispatcher clear information about the person's condition and location.
- Stay on the line for further instructions.
3. Administer Naloxone (Narcan)
- If available, use naloxone, a life-saving medication that reverses opioid overdoses.
- Follow the instructions for nasal spray or injection.
4. Perform Rescue Breathing & CPR if Needed
- If the person is not breathing, tilt their head back, pinch their nose, and give one breath every 5 seconds.
- If they do not have a pulse, start chest compressions.
5. Stay with the Person
- Monitor their breathing and pulse.
- If they start to wake up, keep them calm.
- If there is no improvement within 2-3 minutes, give another dose of naloxone.




How to Get Naloxone
Horizon offers free naloxone and a one-hour virtual REVIVE! training that teaches participants how to recognize and respond to an opioid overdose. Carrying naloxone and knowing how to use it can help prevent fatal overdoses in our community.
Free naloxone is also available at local health departments. Please call ahead to check for availability.
Knowing what to do in an overdose situation can save a life. By carrying naloxone and understanding how to respond, you can make a difference in our community.
